Stages and diagnosis of type 1 diabetes

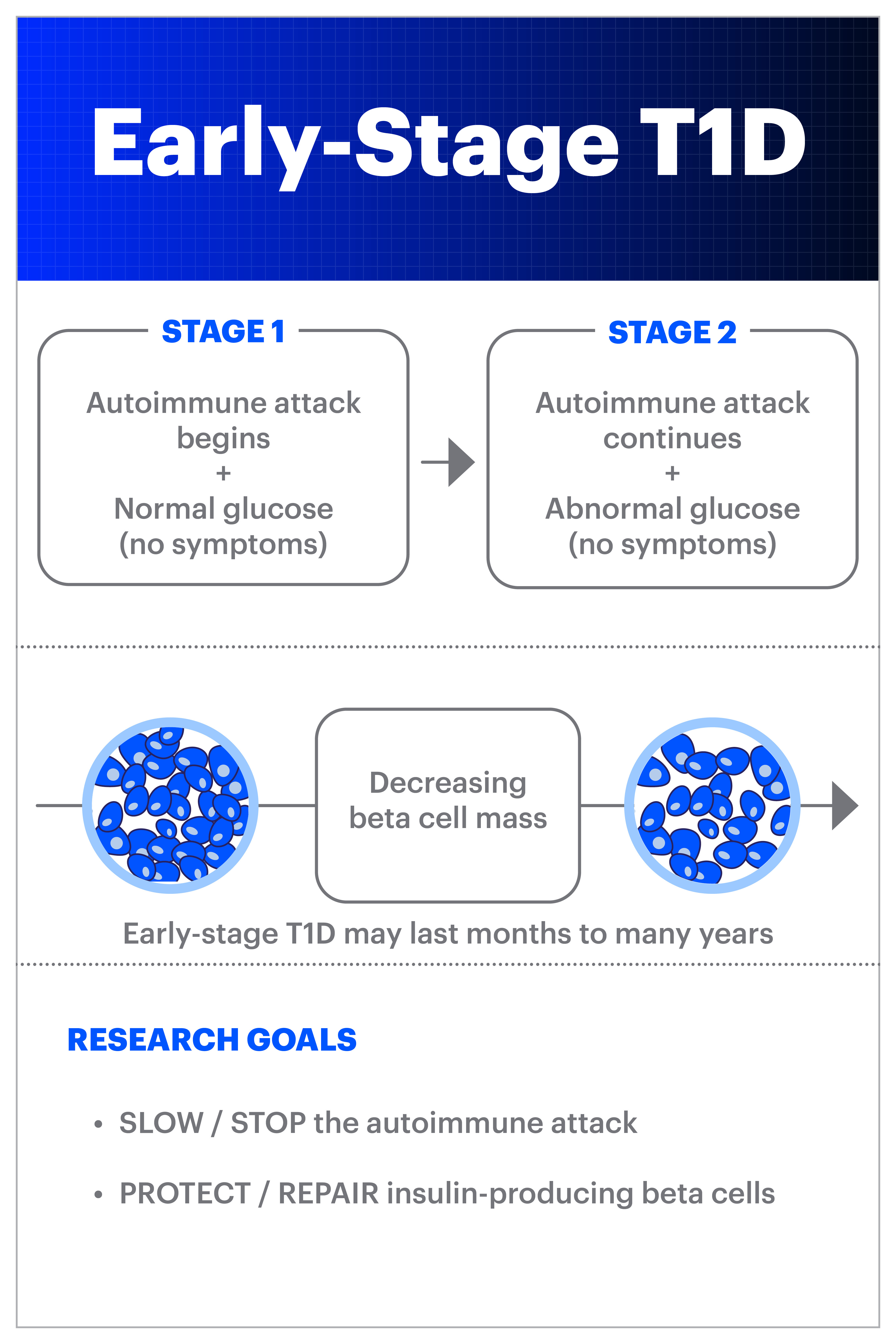
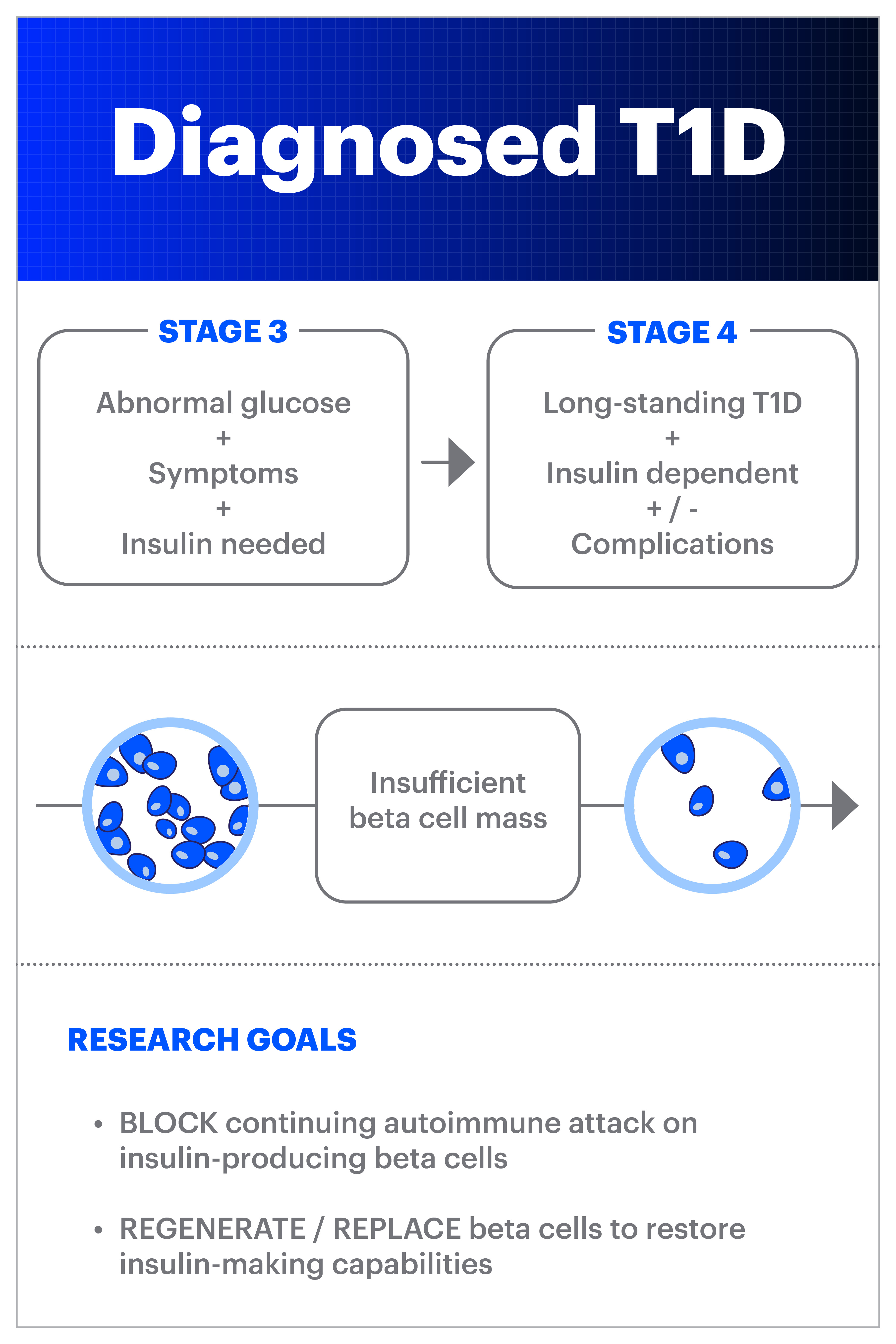
A type 1 diabetes (T1D) diagnosis can happen suddenly and unexpectedly. Many times, particularly in children, the disease might first appear to be like a bad cold or flu. And many adults don’t know that T1D can be developed in adulthood, so they nor their healthcare providers will immediately consider T1D as a possibility when exhibiting symptoms. What we now know from research over the past decade or two is that the autoimmune process is ongoing in the body for months or years before diagnosis. This is now referred to as ‘early stage T1D’ (or stage 1 and stage 2):
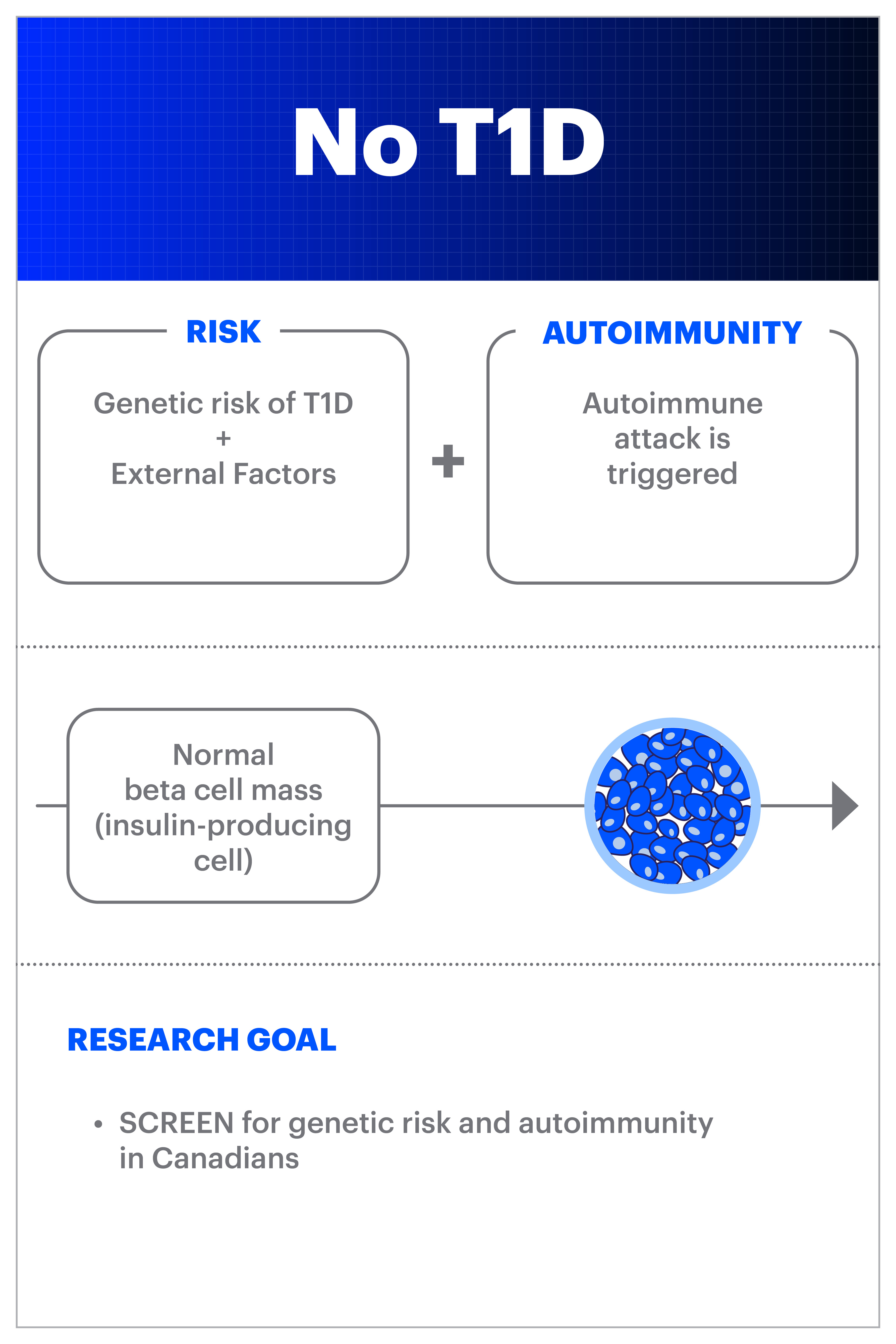
Screening for type 1 diabetes risk
Screening offers the potential to identify people who have early-stage, pre-symptomatic T1D through a blood test. This test identifies the presence of autoantibodies, which are created when the immune system starts attacking the insulin-making beta cells in the pancreas. If a person has two or more persistent autoantibodies, they are at high risk of developing type 1 diabetes.
The only option for T1D screening in Canada is for first- and second-degree relatives of someone with type 1 diabetes through TrialNet. However, only 10-15% of newly diagnosed individuals have a family history, so familial screening alone will miss over 85% of new cases.
Therefore, Breakthrough T1D Canada, in collaboration with CIHR, funded the CIHR-Breakthrough T1D Type 1 Diabetes Screening Research Consortium. This $12 million grant will develop a single nationally coordinated research network to explore key research questions about the feasibility and acceptability of general population screening for early-stage T1D in Canada. The consortium will build on experiences from other countries with T1D screening research programs including the US, UK, Israel, Australia, and multiple European countries.
Learn more: https://breakthroughT1D.ca/canscreent1d-screening-research-consortium-in-canada-announced/
What are the signs and symptoms of type 1 diabetes:
With or without screening, it is important to always be watching for key symptoms of type 1 diabetes. These are often referred to as the 4 T’s:
- Thirsty
- Toilet (frequent urination, possibly bed-wetting in a toilet-trained child)
- Thin (losing weight without trying)
- Tired (fatigue and lethargy)
Other symptoms might include:
- Increased appetite
- Dry mouth
- Blurred vision
- Slow healing cuts and bruises
- Irritability
T1D often initially presents itself with the above symptoms, but it can only be properly identified through a series of tests. It’s important for healthcare providers to be aware of the signs and symptoms of T1D, as often people are only diagnosed at the point of diabetic ketoacidosis or DKA. DKA is a serious life-threatening condition that needs immediate treatment. Ketones and glucose can rise to very high levels in the blood, causing fluid loss and potentially organ failure.
How is type 1 diabetes (T1D) diagnosed?
Fasting blood-glucose test
Doctors will often recommend a fasting blood-glucose test when they suspect T1D in a patient. This is a small sample blood test typically conducted in the morning after fasting overnight. Fasting helps give doctors a clear look at how the body manages blood glucose levels without the impact of food intake.
Oral glucose tolerance test
The oral glucose test takes the fasting test one step further. After fasting and having an initial blood test, people drink a highly sugary drink and then have their blood glucose levels tested over the course of approximately two hours. This shows the benchmark glucose levels without outside food or drink, or activity influences and later measures how the body responds to carbohydrate (sugar) intake.
Random blood-glucose test
The quickest option for testing for T1D is a random glucose test. This test simply measures a patient’s current blood glucose regardless of when and what they most recently ate. On occasion, this will be the first test, and then doctors will elevate to tests noted above as needed.
Glycated hemoglobin (HbA1c) test
The most comprehensive test is the hemoglobin A1c test. This blood test shows the average blood glucose level of the individual for the past two or three months.
C-Peptide
This test measures how much C-peptide is in a person’s blood. Peptide levels typically mirror insulin levels in the body. Low levels of C-peptide and insulin can point to T1D. This is not commonly tested in clinical practice.
Autoantibodies
These are the same autoantibodies that are tested for T1D risk screening. They indicate that an autoimmune attack is present. Autoantibody testing may be ordered to differentiate between type 1 (autoimmune) and type 2 diabetes. However, not everyone with type 1 diabetes will have autoantibodies present at diagnosis.
- Insulin Autoantibodies (IAA)
This tests looks for the antibodies targeting insulin. - Insulinoma-Associated-2 Autoantibodies (IA-2A)
This test looks for antibodies mounted against a specific enzyme in beta cells. Both the IA-2A and GADA tests are common T1D antibody tests. - Zinc Transporter 8 (ZnT8Ab)
This test looks at antibodies targeting an enzyme that is specific to beta cells. - Islet Cell Cytoplasmic Autoantibodies (ICA)
Islet cells are clusters of cells in the pancreas that produce hormones, including insulin. This test identifies a type of islet cell antibodies present in up to 80 percent of people with T1D. - Glutamic Acid Decarboxylase Autoantibodies (GADA or Anti-GAD)
This test looks for antibodies built against a specific enzyme in the insulin-producing pancreatic beta cells.
The honeymoon phase and treatment
After beginning insulin therapy at diagnosis, many people with T1D enter a “honeymoon phase”. The introduction of exogenous (external) insulin gives existing beta cells a break from the constant stress that they have been under for months or years. This can provide a few months to a year of low exogenous insulin requirements and minimal symptoms as the remaining beta cells continue to function normally and produce enough insulin for blood glucose management.
Eventually, the majority of the insulin-producing beta cells in the pancreas cease functioning and the diabetes symptoms return. At this point, exogenous (external) insulin will be needed daily, either by multiple daily injections, pen or insulin pump.
No matter how good A1C or blood glucose tests are during the honeymoon phase, the disease is still present and killing beta cells in the pancreas responsible for producing insulin. During this phase, healthcare providers will work with the individual or family to help maintain blood glucose levels with low-dose insulin treatments. Eventually, the remaining healthy cells will not be able to support the body’s insulin needs and exogenous insulin dosages will need to be increased.
T1D is fairly predictable with regard to endocrine system function during the honeymoon phase, but every case varies just a bit. Paying close attention to the body’s responsiveness to insulin therapy paired with regular blood glucose testing is paramount to successful management.
Slowing the autoimmune progress of type 1 diabetes
Screening for early-stage T1D and understanding how the autoimmune process attacks beta cells provide an opportunity to create therapies to delay, or maybe even prevent, the progression of type 1 diabetes. Breakthrough T1D is currently funding research, some of which is in the clinical trial stage for drug therapies that can slow the autoimmune process or protect beta cells from attack.
Teplizumab (brand name Tzield) was approved by the FDA in 2022 for use in stage 2 T1D to delay the progression to diagnosis. This is not yet available in Canada.
In a Breakthrough T1D-funded clinical trial, baricitinib—a small molecule immune therapy that blocks Janus Kinase, which is critical to signaling pathways within both immune cells and beta cells in T1D—preserved beta cell function in individuals newly-diagnosed with T1D .
Additionally, ustekinumab, in another Breakthrough T1D-funded trial currently recruiting in Canada, is helping Breakthrough T1D address the autoimmunity behind T1D.
Ultimately, the hope is that T1D screening will be a pathway to a cure, catching the disease and treating it before it can start.
