Approximately 300,000 Canadians live with type 1 diabetes (T1D), an autoimmune disease that destroys the cells in the pancreas responsible for making insulin. The discovery of the insulin hormone over 100 years ago meant the first treatment for the disease, whereas previously a diagnosis meant certain death. But a century later, it remains the only treatment.
On April 4, 2022 to publicly launch JDRF’s $100M Campaign to Accelerate, five brave Canadians will become Leaders in History, as part of JDRF’s Let’s Make History Again fundraising event.
For 100 hours, they will live atop of a flagpole in their respective cities. The event celebrates the 100th anniversary of the first successful injection of insulin, which took place in January 1922. The goal of this flagship fundraising event is for our Leaders – along with supporters across Canada – to raise a collective $15M and get us closer to our goal of a future without T1D.
Dexcom, a longtime supporter of JDRF, once again stepped up to be an event sponsor. The significance of the 100th anniversary was particularly meaningful to the organization, which has been on the forefront of diabetes innovation with their continuous glucose monitoring (CGM) technology. The Dexcom G6 CGM System is used by many of the event participants who have T1D.
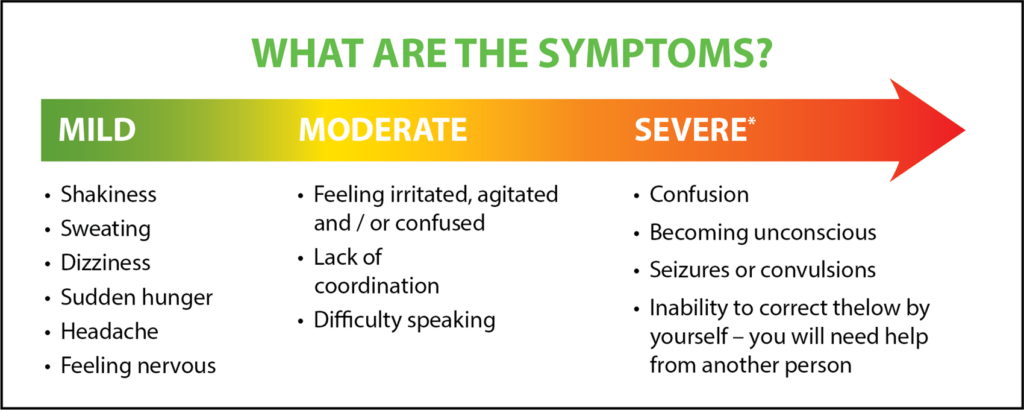
The body is ever-changing and the factors that affect glucose levels are not necessarily predictable, including sleep, stress, hormones, physical activity, medication, other medical conditions.
To maintain health and vitality and longevity, keeping glucose levels in range is essential – and this requires careful monitoring to manage the delicate balance of insulin and those other factors, as they occur. With other complementary technologies like insulin pumps and advancements with insulin, management of T1D can become easier on individuals and their families.
How type 1 diabetes management has progressed
Evolution of insulin – People with T1D now have access to both long-acting and short-acting insulins, which can offer a little more flexibility in life. Before these types of insulins, someone living with T1D would have to keep a repeatable routine with the same amount of insulin, activity, and same proportion of food/carbohydrates at the same time every day.
Glucose monitoring – Before finger prick tests and advanced glucose monitors, one would need to urinate on a stick and could only get a vague idea of whether their glucose was high or low. Early forms of blood glucose meters took a sample of blood, and then one would have to wait to get results – at first a few minutes and then eventually a few seconds. This could still prove difficult, especially for parents with young children. Constant finger pricks were painful, and it was challenging to get a sense of blood sugar trends or to have any idea of time in range.
Now, with glucose sensors – the user can develop a greater understanding of their own glucose trends and make more informed insulin dosing and treating decisions. This also has the benefit of helping to prevent a severe hypoglycemic event – and that is life-changing. With remote monitoring now also possible (for parents, caregivers & others) through apps like the Dexcom Follow App, it has changed life for the entire family.
Insulin pumps – These pumps used to be approximately the size of a backpack and evolved over time along with insulin and the kind of precision engineering needed to be able to deliver small increments of doses that the individual could control. Now, they are about the size of a cell phone or even smaller, and allow the individual to fine-tune their insulin dosing more precisely for tighter control and easier corrections. With the added capability of being able to decrease or increase basal rates or extend boluses to release over time, the individual has the power to better approximate what a functioning pancreas might do.
Now, with insulin pumps that are integrated with continuous glucose monitoring sensor technology – insulin delivery can be automated to an extent. While active diabetes management is still necessary, the burden on the user is significantly less than it used to be.
In 2022, diabetes technology isn’t just better – quality of life is demonstrably improved with access to these devices. There is less wondering. One can check their glucose levels at a glance and know if it’s time for a snack or rest, or if something else is going on. And the burden on parents is significantly reduced. Before advanced glucose monitors, monitoring was reliant upon a child to track their glucose themselves with a blood glucose meter, recording results in a logbook. Now, with sensors and remote monitoring – parents can see what’s happening on their phone and intervene if necessary for a child’s safety. It improves peace of mind for the entire family.
For people living with T1D, better disease management is now possible with less effort. And with better control – one feels better and healthier – and this allows life to open. JDRF’s #AccessForAll campaign aims to make type 1 diabetes (T1D) technology affordable and accessible for everyone living with this disease, by working with the T1D community in their efforts to increase public and private coverage for insulin pumps and advanced glucose monitors (CGM and Flash GM).
Dexcom has always been a strong supporter of JDRF, and we serve the same community of individuals and families grappling with type 1 diabetes. Many of the Dexcom staff themselves live with the condition, and until there’s a cure – the company aims to make things better with tools to empower people to take control of diabetes. Research is increasingly promising, and an event like Let’s Make History Again can go a long way in getting attention for this important cause and for the T1D community.
JDRF thanks Dexcom for its significant contribution to our Let’s Make History Again event. It is with the support of important corporate partners that we can fund the most promising T1D research and get closer to our goal of a world one day free from type 1 diabetes. Until that time, advanced diabetes technology makes living with T1D day-to-day easier and better.
To learn more: www.canadacuresdiabetes.ca